The shoulder is the most mobile joint in the body; this makes it the easiest joint to dislocate. A dislocated shoulder occurs when the upper arm bone separates from the socket in your shoulder blade.
The most common type of shoulder dislocation is the anterior shoulder dislocation (much more common than posterior shoulder dislocation) which occurs when there's a sudden blow to your shoulder causing it to forcefully rotate, extend or abduct and cause the top of your shoulder bone to dislocate for the shoulder blade.
Causes of Anterior Shoulder Dislocation
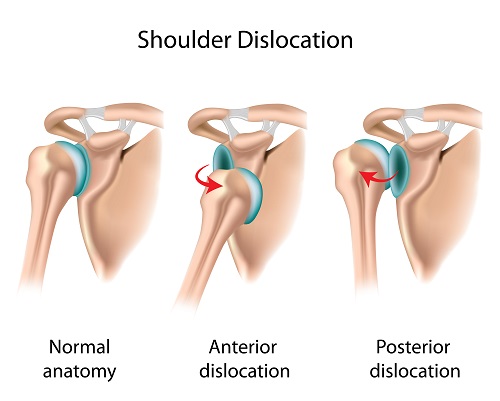 The humeral head, better known as the top of the shoulder (humerus) bone will end up lying anterior, medial, or inferior to its normal location and the glenoid fossa. Where it ends up lying determines which of the four types of anterior shoulder dislocation has occurred. The four types are the subcoracoid (which is the most common), subglenoid, subclavicular, and intrathoracic (which is the least common).
The humeral head, better known as the top of the shoulder (humerus) bone will end up lying anterior, medial, or inferior to its normal location and the glenoid fossa. Where it ends up lying determines which of the four types of anterior shoulder dislocation has occurred. The four types are the subcoracoid (which is the most common), subglenoid, subclavicular, and intrathoracic (which is the least common).
Dislocating a shoulder bone takes a lot of force; however, extreme over rotation may also pop it out of place. Sometimes a partial dislocation may occur which happens when the upper humerus bone is only partially out of the shoulder socket.
The top three most common causes of anterior shoulder dislocation are:
- High impact sports: In sports such as football and hockey which rely on high levels of contact, it is common for someone to incur a shoulder dislocation. Sports that are commonly known for the athletes to take hard falls such as skiing, gymnastics, and volleyball may also result in a dislocated shoulder.
- Traumatic accidents: Other traumatic accidents such as motor vehicle accidents also have a high result rate for anterior shoulder dislocation.
- Falling: Shoulder dislocations are also very common in patients who have fallen off a ladder, down the stairs, or fallen simply because they tripped over the rug.
Who Is at Risk
Anterior shoulder dislocation mostly occurs in young men who sustain high impact injuries to the shoulder, whether it's through accidents or impact sports. Older adults are the second largest group of patients who sustain this type of injury. In the older adults it is usually an isolated event caused by a lower impact event.
Diagnosis of Anterior Shoulder Dislocation
Most of the time, your doctor or physiotherapist can diagnose your shoulder dislocation right in the clinic. After discussing your symptoms, how the injury occurred, and any other injuries you may have sustained, your doctor will check your shoulder. When they do this, they are looking for signs of instability and dislocated shoulder. If you play on a sports field, generally the medical personnel on the field can diagnose it there.
Once a shoulder dislocation diagnosis has been made, your doctor may request imaging tests to confirm their diagnosis. X-rays, magnetic resonance imaging (MRI), and magnetic resonance arthrogram (MRA) tests will confirm the diagnosis plus aid in discovering any fractures, legions, or tears that may have occurred along with the dislocation.
Treatment of Anterior Shoulder Dislocation
A closed reduction and immobilization are the two main methods used to treat anterior shoulder dislocations. Once the shoulder bone has been placed back into the socket, it is important that you allow 6 weeks for proper healing.
1. Closed Reduction
When you go to the doctor, he or she would try to get the dislocated shoulder back into place with gentle and helpful maneuvers. To help with the pain, you may be given sedative, muscle relaxant or even general anesthetic before the process based on the degree of the swelling and pain. As soon as your bones get back to a proper position, the pain you experience would improve greatly.
2. Immobilization
This means that you are going to need to keep your shoulder immobile as much as possible. To do that, the doctor may use a sling or splint to immobilize your shoulder. As for the time that you need to wear that, it depends on when the sling is applied and the condition of your dislocated shoulder. But eventually you will begin to slowly use your shoulder again.
3. Surgery
Most of the time, surgery is not required; however, there are times that the extent of injuries do require surgery for adequate repair. These instances include:
- Instability of the shoulder: When there is damage to the inferior glenohumeral ligament, you will not be able to properly stabilize your shoulder without surgery.
- Lesions are discovered: Hill-sachs lesion, bankart lesion, or other anterior glenolabral injuries need to be repaired by surgery. These occur when there are fractures caused by the humeral head coming out of the socket.
- Other damage occurs: When the axillary artery or the brachial plexus are damaged during the dislocation it is vital that you receive surgery to repair the damage. It is also essential to use surgery when there is intraarticular loose body evident.
4. Exercises
Once you are able to begin using it again, you will work with a physical therapist who will create an exercise plan to strengthen your shoulder. This plan will help you maintain your mobility and reduce muscle waste while you heal. The exercise plan will most likely begin with a series of isometric exercises which do not require your shoulder to move.
Will I Dislocate My Shoulder Again?
Yes. You will most likely experience a shoulder dislocation again. The chance of a repeat occurrence does diminish as you age, but those who are under the age of 25 have an 80% chance of reoccurrence. Due to this high percentage of recurrence, the main purpose of treatment is to help reduce the chance of dislocating your shoulder again.
After you have dislocated your shoulder twice, you will most likely experience frequent dislocations. They will occur every time you put your shoulder into a specific position; each time it will require less and less force.
Then How Can I Avoid Reoccurrence?
The best way to avoid dislocating your shoulder again is to follow your doctor's recommendations and keep your arm in a sling for 6-8 weeks, or more, and proceed with your physical therapy plan.
If you are an athlete, your doctor is going to recommend that you wait up from 8-12 weeks before resuming the activity. Even following the plan of immobilization and physical therapy, you still risk having an anterior shoulder dislocation again. By resuming activity within the first three weeks of treatment the risk is even higher.
