A fibrous cortical defect is common benign (non-cancerous) tumor in the bone that affects up to 40 percent of children and is most common in adolescents. It is also known by other names likenon-ossifying fibroma (NOF), a term which is often used when the tumor or lesion is large and encroaches upon the central part of the bone called the medullary canal. Other terms used include fibroxanthoma, benign fibrous histiocytoma, and non-osteogenic fibroma.
What Are the Symptoms of Fibrous Cortical Defect?
A fibrous cortical defect is a benign bone lesion that is often detected on radiologic or x-ray examination. This is a developmental defect in which some part of the bone is filled with fibrous, instead of bone tissue. It is therefore sometimes called a non-ossifying fibroma because of failure of part of a bone to ossify, or develop into bone tissue. It commonly affects the metaphysis, or the end of a long bone, such as the femur (thigh bone) or the tibia (lower leg bone). Most of the time, the lesion eventually ossifies and undergoes remodeling, resulting in dense areas of the bone, but sometimes the lesion may also enlarge. Children and adolescents are often affected.
A small fibrous cortical defect is usually asymptomatic and may only be detected incidentally on x-ray examination. However, if it is large enough to affect about half of the bone’s diameter, it may cause pain and increase a child’s risk of sustaining a pathologic bone fracture.
Presentation on X-Ray
Non-ossifying fibromas may appear as a single, oblong shaped translucent lesion (uniloculated) with well-defined borders on x-ray which has a diameter of less than 2 cm, but they may also appear multiloculated (with many holes). If the lesions are associated with other features like café au lait spots, moles or nevi, hypogonadism (sex glands produce little or no sex hormones), mental retardation, and other abnormalities in the eyes and the heart, the diagnosis may be called Jaffe-Campanacci syndrome.
When to Worry
Children who do not manifest any symptoms usually do not need treatment. However, if the fibrous cortical defect affects a bigger part of the bone, becomes very painful, and increases their risk for pathological fractures, prophylactic surgery may be recommended to stabilize the bone.
Here are some images depictingfibrous cortical defect:
This is plain radiograph showing a fibrous cortical defect in the upper end of a leg bone (proximal tibia).

This is a lateral radiograph view demonstrating a unilocular fibrous cortical defect in upper end of a leg bone (proximal tibia).

This radiograph shows a larger lobulated fibrous cortical defect located in the lower end of the leg bone (distal tibia).

The four images show the different stages of ossification (sclerotization) of non-ossifying fibromas (Ritschl’s classification). Stage A (left upper) shows a single oval lesion with smooth outlines. Stage B (upper right) shows the polycyclic borders of a lesion. Stage C (middle right) shows a lesion that is partially calcified (ossified). Stage D (lower right) shows a completely ossified (sclerotic) lesion.
The image on the left shows a smallfibrous cortical defect in the upper portion of the leg seen in a 7-year old girl. The image on the right shows a larger non-ossifying fibroma protruding into the central bone (medullary) cavity, which was found in the lower portion of the leg of a 12-year old patient.
This is a non-ossifying fibroma as seen on CT scan. Left (A), axial image of a small, non-ossifying fibroma (stage B) seen in the upper arm (humerus), and the same lesion in sagittal and coronal views (B and C, respectively).

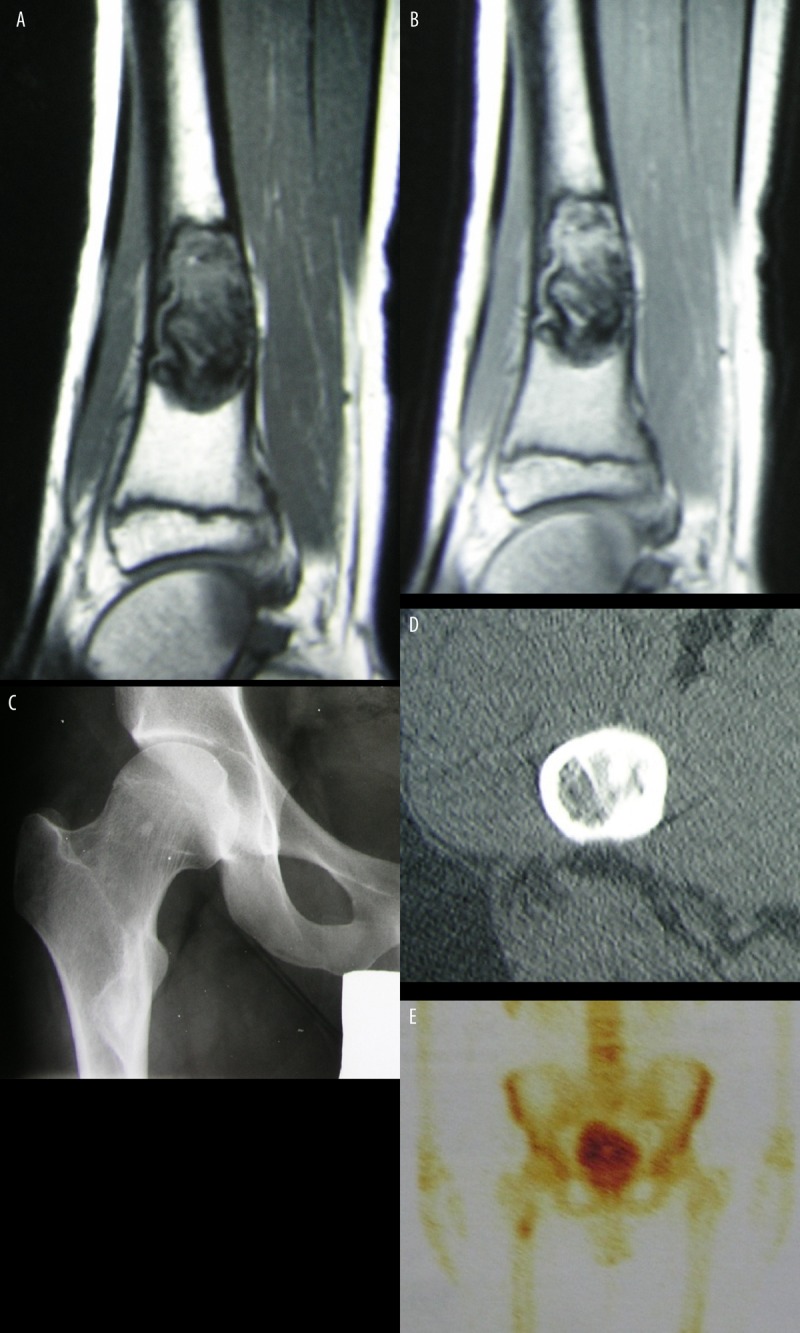
These MRI and scintigraphic images show a fibrous cortical defect, revealing a heterogeneous, low signal intensity (A) that is enhanced after administration of IV contrast medium (B). Images C and D show a non-ossifying fibroma found in a 21-year-old man, in his upper thigh bone (proximal femur). Image E shows a slight increase in accumulation of a radioisotope within the lesion on bone scan. (Images by Joanna Mączewska, MD, Department of Nuclear Medicine, Medical University of Warsaw).
Treatment s for Fibrous Cortical Defect
Most of these lesions are benign and self-limiting so usually no treatment is needed, however, as mentioned above, in severe cases, treatment is essential and medical advice should be followed.
Medical Treatment
Pathologic fractures in children are usually treated by casting to avoid injury to the metaphyses during surgery. If the fibrous cortical defect does not regress in spite of fracture union, curettage and bone grafting may be necessary.
Surgical Treatment
Unstable fractures must be treated surgically, as well as lesions with high risk of pathologic fracture. This involves bone curettage with grafting.
Complicationsof fibrous cortical defect surgery
Possible complications of surgery include injury to the adjacent metaphysis, which can result in growth abnormalities.
Follow-up
Patients with typical lesions require only one follow-up examination with radiograph 6-12 weeks from diagnosis. A fibrous cortical defect usually ossifies at puberty. However, patients with large lesions must be followed every 4-6 months to evaluate progression of lesion size. Patients must be advised to avoid engaging in too many activities, especially contact sports, to prevent fractures.
Following a fracture, the involved extremity must be immobilized until radiological evidence of union is observed. If the lesion does not regress and risk of another fracture is high, curettage may be indicated, with or without doing internal fixation and bone grafting.
Outcome / Prognosis
A fibrous cortical defect usually regresses with time. Prognosis is excellent even in patients who require curettage and bone grafting.
